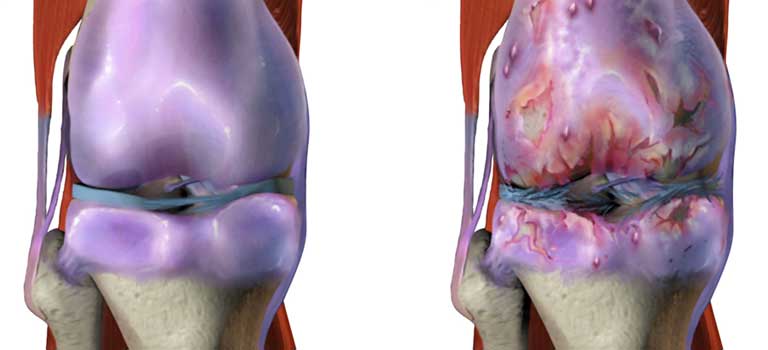
Osteoarthritis (OA) is an extremely common condition which can affect any of the joints simply by chronic “wear-and-tear” from normal aging also known as degeneration or degenerative joint “disease”. The knee joint is consists of bones which come together and move similar to a hinge. The bones are separated by protective cartilage. However, the cartilage wears away which may eventually lead to bone rubbing directly on bone. The joint then becomes stiff, painful or swollen. Other symptoms may include snapping, clicking or locking of the joint. It may be more painful first thing in the morning or after prolonged periods of immobility or activity as well as with inclement or changing weather.
The most commonly affected are weight-bearing joints such as the knee and hip, but also the hand especially basal thumb joints. Previous injury or surgery to a joint such as arthroscopic meniscectomy for a knee meniscus tear may hasten the onset or progression of OA. X-rays are usually the best diagnostic test to detect the presence of knee OA. MRI is more useful in looking at the soft tissue structures such as tendons, ligaments and the meniscus.
The treatment of knee osteoarthritis (OA) could include medications, non-pharmacologic therapies such as heat, cold or electrical stimulation, physical therapy, splints or other joint aids and weight loss. Ultimately, injections and surgery may be potential treatment options. Since each one of these nonoperative treatments provides only modest benefit, a multi-modal approach is recommended.
Related Articles
- Knee Pain Treatment: Viscosupplementation Injections
- Osteoarthritis (OA) – Arthritis Treatment Options – Injection Therapy – Part II
- A Non-Surgical Treatment for Osteoarthritis (OA) | Genicular RF Neurotomy
- Orthobiologics in the Treatment of Knee Osteoarthritis
Medications
Over-the-counter medications such as Acetaminophen, Ibuprofen, and Naproxen can be used. Only if these medications do not provide sufficient relief should prescription medications be considered. These prescription medications include other oral or topical non-steroidal anti-inflammatory agents (NSAIDs) or COX-2 inhibitors (celecoxib). Glucosamine with or without chondroitin may also be used. However, this medication needs to be taken for several months before reaching conclusions about its efficacy. Scientific studies have shown variable benefit from this medication depending upon the area affected by the OA, but have not shown to decrease or reverse progression of arthritis.
Injection Therapy
In the past, injection therapy was limited to essentially only corticosteroids (steroids). However, there are now several other options.
Steroid Injections:
If symptoms are severe or not controlled by the more conservative options, an injection of steroid can be tremendously beneficial. The steroid is used to decrease any inflammation associated with the painful joint. Although OA is not considered to be a significantly inflammatory condition, medical evidence suggests an inflammatory component to the condition. Corticosteroids however will NOT slow the progression of OA.
Patients frequently express concern regarding the use of steroid. However, if used in a clinically appropriate manner, steroids can be therapeutically beneficial while minimizing the potential adverse effects. If a patient is diabetic, a corticosteroid will increase the serum glucose (blood sugar) levels generally for no more than 48-72 hours. Adjustments in the diabetic medication may control this temporary blood sugar elevation. Other adverse effects of corticosteroids include toxic effects to the joint cartilage. If used excessively, corticosteroids have been associated with temporary elevations in blood pressure and accelerated bone thinning.
Viscosupplementation:
Viscosupplementation refers to the injection of hyaluronic acid (HA)-derived preparations into the affected joint. There are several preparations available. Generally, the injections are done on a weekly basis for 3-5 visits. The use of viscosupplementation is only indicated for use in knee osteoarthritis and therefore insurance coverage could be limited when treating other joints. There has been recent medical controversy over the efficacy of HA injections, which continue to be used on a regular basis clinically. The HA injections are felt to be beneficial in maintaining joint health without the adverse effects of corticosteroid.
Orthobiologics (PRP and Stem Cells/BMA):
Due to the limited effectiveness of surgical (arthroscopy or arthroplasty) and non-surgical therapies, regenerative medicine therapies (orthobiologic agents) have become increasingly used, researched and studied as a potential alternative for many arthritic conditions, not just to treat the symptoms, but also potentially slow the progression of the disease. Research has shown some benefit of PRP over the use of steroids and HA injections in terms of long-term pain reduction. Little is known about how treatment with PRP and stem cells actually work with limited studies available, therefore these treatment options remain “investigational.” Most PRP and stem cells are autologous (obtained from the patient’s own blood or bone marrow) therefore the procedure is considered a relatively safe option with limited complication or adverse reactions.
Other Nonsurgical Treatment Options for Knee Osteoarthritis
Genicular RadioFrequency (RF)
– If surgical (knee replacement or arthroplasty) or nonsurgical treatments fail to provide the necessary benefit, genicular radiofrequency (RF) is yet another treatment option. In summary, the use of injections in the treatment of knee OA is an integral part of the multi-modal treatment approach for this condition. There are several injection and nonsurgical interventional options available. Generally, these options will be less effective in more severe joint arthritis, but can be helpful not only in relieving pain, but slowing the progression of the OA.