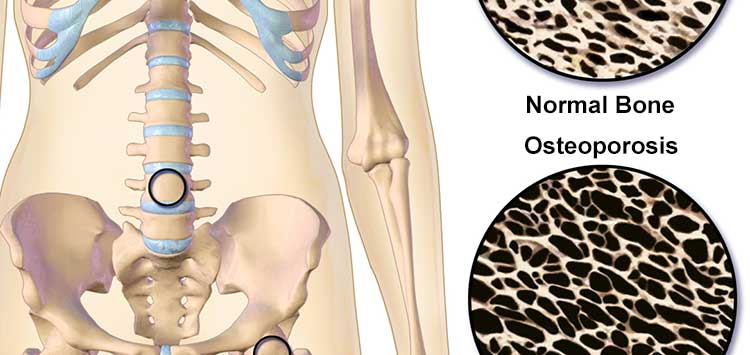
What is Osteoporosis?
Osteoporosis is a bone disease in which overall bone mass is decreased and the bone becomes more porous. As bones become more porous, the risk of a fracture greatly increases. Unfortunately, like many silent diseases such as diabetes and hypertension, osteoporosis sometimes is not diagnosed until after a complication. In the case of osteoporosis, this means a compression fracture.
What is a Compression Fracture?
A compression fracture is a collapse of the bones of the spine called vertebrae which commonly occurs in the setting of osteoporosis. In the most severe cases, fragile bones from osteoporosis can fracture from minimal force, such as a sneeze or simply bending forward. In other cases, a fracture can occur from a fall which otherwise would not have resulted in fracture if healthy, non-osteoporotic bone was present.
Compression fractures occur in about 25% of people over 70 years old and in about 50% of people over 80 years old. Peak bone mass is established in both men and women at about the age of 30 years old. After this, the density of our bones gradually decreases over time.
Symptoms of Vertebral Compression Fracture
The most common symptom after an acute compression fracture is pain at the site of injury, that is, back pain. Patients may also complain of pain with bending or twisting. A forward curvature of the spine and loss of height can occur after compression fractures in multiple vertebrae. Difficulty breathing may occur in patients with a past medical history of respiratory illness, such as asthma or chronic obstructive pulmonary disease (COPD).
Risk Factors for Osteoporosis and Compression Fracture
- Postmenopausal
- Female gender
- Caucasian or Asian race
- Recent extended bed rest
- Tobacco use
- Chronic steroid treatment
- History of previous fracture
Diagnosis of Vertebral Compression Fracture
A careful history and physical exam are first completed. A thoracic and lumbar x-ray are obtained to look for vertebrae with decreased height. This is then correlated to the area of pain and duration of symptoms. An MRI of the spine can also be completed to look for bone edema (a sign of acute injury), which would allow certain procedures to be done for pain relief. Imaging will also help rule out other causes, such as bone tumors.
Vertebral Augmentation
Two types of vertebral augmentation are presently available, kyphoplasty and vertebroplasty. These treatments are used to decrease pain and stabilize compression fractures. The initial 6 weeks after a compression fracture are first managed with conservative care including bracing and pain medication. Some uncomplicated spinal fractures may heal on their own.
A vertebroplasty is an outpatient procedure in which bone cement is injected into a specific vertebrae. For those with severe disabling pain, this procedure may allow a patient to resume normal activities faster and decrease the amount of daily pain medication needed. Studies have shown that when compared to conservative treatment, vertebroplasty reduces pain as well as overall disability.
A kyphoplasty is also an outpatient procedure that attempts to stabilize the fractured vertebrae by using bone cement. However, this procedure differs by first using an inflatable balloon to create a cavity and partially restore the bone’s original shape prior to placing the cement. Studies have also shown that kyphoplasty has been linked to improved pain and reduced need for pain medication.
Most importantly, whether the fracture heals on its own or with vertebral augmentation, the underlying osteoporosis needs to be treated to help prevent future fractures.