The Anatomy of a Disc
The disc is like a jelly doughnut. There is jelly on the inside, known as the nucleus pulposus. The doughnut part is made up of strong, fibrous bands around the outside that surround and contain the jelly, known as the annulus fibrosis. Together they act as a shock absorber between the vertebrae to allow movement and provide cushioning.
What Can Go Wrong With a Disc?
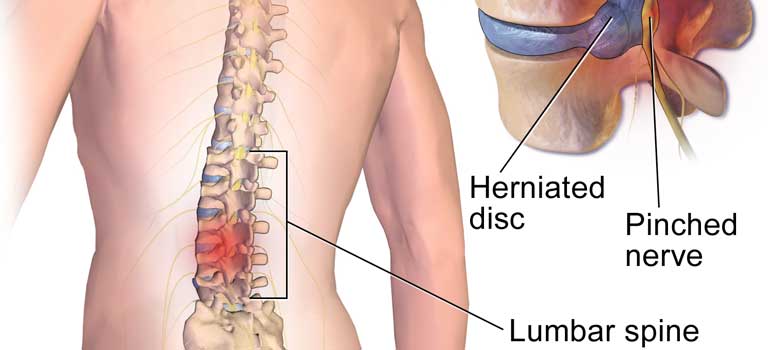
During an injury (bending, lifting, twisting, falling) a disc can either herniate or internally disrupt (Internal Disc Disruption). A herniated disc means the nucleus pulposis or “jelly” is bulging through the annulus and bulges outside of the normal space it sits in. With strong supporting ligaments in the front and back of the spine, the disc usually bulges out the side, sometimes pinching a nerve. A nerve being pinched usually results in “sciatica” or leg pain.
An internally disrupted disc means the disc may tear through the fibrous layers of annulus and the “jelly” can leak out of its contained space. There are nerves embedded within the annulus fibers which may become highly irritated by the jelly substance causing what is referred to as “discogenic” or low back pain. Some people will also experience what is considered “referred” pain into one or both legs. Discogenic pain is considered to be the most common cause of chronic low back pain; especially in the “working age” population. Occasionally both situations may happen simultaneously within the same disc.
How Do I Know if That Is What I Have?
If pain persists long-term, usually 6 months or greater, and other causes of low back pain are ruled-out (facet joint pain, vertebrogenic pain, muscular pain, sacroiliac joint pain), a diagnosis of discogenic pain is usually suspected. MRI may mention the possibility of annular tear or fissure, but the best definitive way to diagnose disc pain is through discography.
How Do I “Fix” It An Internal Disc Disruption?
Unfortunately, treatment options for discogenic pain are limited and rarely result in a “cure.” Discs receive very poor blood supply; therefore do not have the ability to heal themselves. Historically, when people were diagnosed with disc pain, they would decide to either live with it, take medications, or have surgery; which were not great options. Long-term medication use could sometimes lead to addiction; and surgery (lumbar spinal fusion) has less than a 50% success rate for pain reduction, but also increases the likelihood of adjacent segment disc issues.
Fortunately, we now have some other options to offer; intradiscal injections of biologic agents. Two main types of biologic agents have been studied for treatment of discogenic low back pain: PRP (Platelet-Rich Plasma) and “stem cells” (MSCs) or BMAC (Bone Marrow Aspirate Concentrate). Both are autologous treatments, meaning they are taken from the patient’s own blood (PRP) or bone marrow (stem cells) making both treatments extremely safe and readily accessible with minimal to no extra manipulation required. Either option can be used independently or together simultaneously. Studies regarding intradiscal injections of PRP and BMAC have both shown favorable outcomes in the reduction of pain long-term, favoring even better outcomes with stem cells/BMAC. Continuous research is still ongoing in this field of medicine, but so far has been promising and has given patients alternative options in an otherwise difficult situation.