Spinal cord stimulation (SCS) has been widely available for decades for the treatment of chronic pain including failed back surgeries, complex regional pain syndrome (CRPS), and various other neuropathic pain conditions. (See articles on: Back Pain and Extremities)
CRPS (Type I and II) is a unique condition that has many challenges when it comes to treatment, including traditional SCS. According to studies, 40-50% of patients with CRPS achieve meaningful pain relief with traditional SCS. It is believed that less than optimal results may be due to the limitations in targeting very specific or focal areas of pain (especially distal extremities ie. knee, foot).
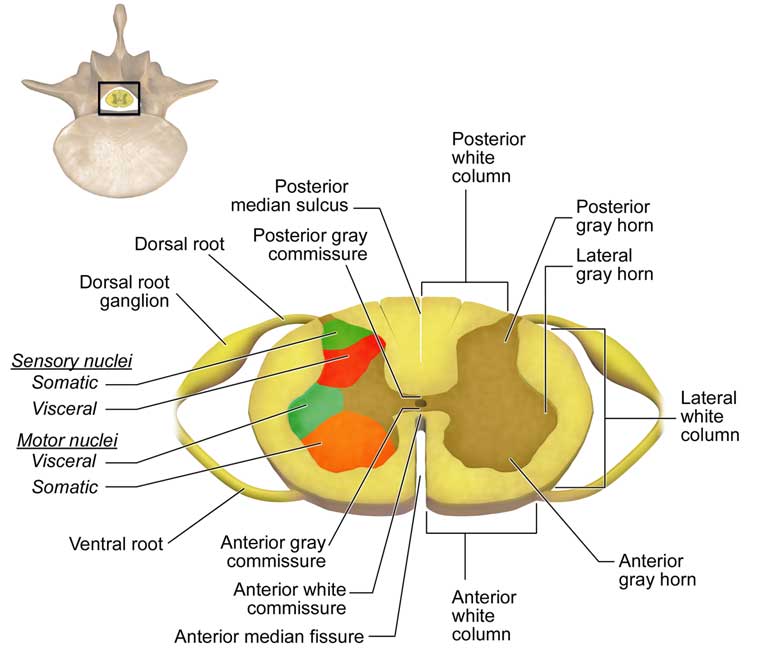
Dorsal root ganglion (DRG) stimulation was first FDA approved in the US in 2016 for CRPS.
The way it works is very similar to that of traditional SCS with several key differences. DRG stimulation is able to provide stimulation to focal areas of pain that have been historically difficult to treat, such as the abdomen, groin, knee and foot. The benefit of concentrating the stimulation to very specific dorsal root ganglions is minimizing stimulation of the rest of the spinal cord, which may be unnecessary for some patients. More effective stimulation can be achieved by requiring much less energy. According to studies, more patients (74% with DRG as opposed to 53% with traditional SCS) showed more significant and sustained pain relief (80% reduction) at 3- and 12- months post implant compared to traditional SCS.
DRG stimulation is primary indicated for focal (localized) neuropathic pain conditions.
Although it was studied and intended for the CRPS Type I and II patient population, it has the ability to treat many other unique chronic pain problems. The possibilities include, but not limited to, postsurgical and/or post-injury groin, knee and foot/ankle pain, abdominal/pelvic pain, phantom limb pains, lumbar radiculopathy, peripheral neuropathy (ie, diabetic neuropathy), postherpetic neuralgia (shingles), and potentially refractory discogenic low back pain.